View this episode's trailer
Episode Description
“I’m coming up on my 50th year anniversary of my time as a science writer, writing almost exclusively about cancer...And I’ll tell you, it gets more and more interesting.”
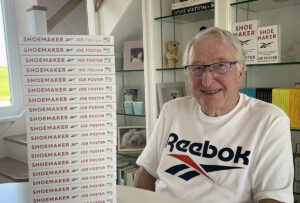
A graduate of NYU and Stanford University, medical writer Dr. Ralph Moss has been independently evaluating the claims of conventional and non-conventional cancer treatment for the past 35 years. But before he began writing books, he helped to leak the truth about an esteemed scientist’s research on a drug that could block cancer metastasis—when his bosses wanted him to lie. [More on that in Part 2!]
In Part 1 of this gripping conversation Dr. Moss talks about getting his start in medical research and writing, landing a job at the prestigious Memorial Sloan Kettering Cancer Center. He sheds light on why oncologists treat patients with “cookbook methods,” the tremendous pressure on doctors not to deviate from medical guidelines and the connection between a doctor’s treatment plan and your insurance company.
His passion for helping people overcome cancer is clear. As a cancer survivor himself, he knows well the importance of his work.
LISTEN TO PART 2 of the conversation to learn THE SHOCKING TRUTH and WHAT IT COST.
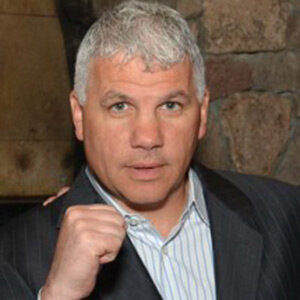
For over 40 years Dr. Gary Onik has been pioneering advances in cancer treatment that have rocked the field of oncology, inventing an entirely new branch of cancer treatment now known as “Interventional Oncology” based on his innovative minimally invasive techniques. Both doctor and patient, he created a cancer vaccine and successfully treated his own terminal prostate cancer using his invention. In addition to his medical practice, Dr. Onik is an Adjunct Professor of Mechanical Engineering at Carnegie Mellon University, working closely with his colleagues to develop the next generation of cancer fighting technologies. His latest work, using immunotherapy to treat metastatic cancer, offers hope to those patients with literally no other options.
TO CONTACT DR. ONIK visit https://www.garyonik.com/.
TRANSCRIPT
Dr. Gary Onik [00:00:00] Hello, I’m Dr. Gary Onik, and I’m your host for Cancer is Tough, but YOU are TOUGHER! I want to thank The Beach Boys for allowing us to use their piece of music that is dear to my heart. My podcast is uniquely personal. I know both sides of the cancer equation. I am a cancer specialist and researcher, as well as a cancer patient and survivor. I will address various treatment modalities in the podcast, but that’s not really what this podcast is about. This podcast is about the unique cancer journey that a patient and their family and friends take when they are diagnosed and treated with this dread disease. We’ll delve into the inner emotional and spiritual resources. Patients and their loved ones need to address their concerns of choosing a treatment strategy that will harmonize with their worldview while grappling with state-of-the-art treatments versus alternative treatments. When I was asked who’s going to be my target audience, the obvious answer was everyone. It’s a rare person that has not had cancer touch their lives, either as a patient, a family member or friend. If you’re that rare person that hasn’t had cancer touch their lives, almost certainly at some point, cancer will drag you into its maelstrom. I hope that you find this show both a resource and a comfort in dealing with your cancer journey.
Dr. Gary Onik [00:02:13] I’d like to welcome Dr. Ralph Moss. He’s the author of the Moss Reports. He’s been helping patients deal with cancer since 1977 through his reports, and he’s also the author of a bunch of books. I don’t know what is the… for more than one book is it a bunch or a gaggle? A herd? You know? I’m not sure.
Dr. Moss [00:02:46] It’s a closet full.
Dr. Gary Onik [00:02:47] It’s a closet full collection. So, you’ve got a lot, a lot of books out there.
Dr. Moss Yeah.
Dr. Gary Onik [00:02:54] Just look on Amazon. It’ll take up half your computer memory. He also has a unique experience because he’s a cancer expert and he’s also a cancer survivor. So, I think he’ll be able to give us a very unique view of the area of cancer and how it relates to a number of very interesting issues. So, I’d like to start with a discussion. Interesting background. I mean, you were trained as a classicist and now you ended up helping cancer patients. How did that happen? If you don’t mind going into the background of that?
Dr. Moss [00:03:38] So what I really wanted was to be a writer. I had almost a compulsion to write. And even, I remember when I was 14, you know, all the other kids were out playing basketball and I was sitting at my typewriter typing away furiously and my next-door neighbor poked his head in the window and said, hey, why aren’t you out there playing with the other kids? What are you doing? Writing your autobiography? And it was very embarrassing because I was writing my autobiography so, fourteen. So, my basic philosophy was, I had the idea and wasn’t an original idea, that the best way, the way to be the best writer that I could be would be to read the best literature that I could read. And I didn’t want to just be an ordinary English major, I wanted to actually learn something that I couldn’t learn on my own. And so, I was drawn to the classics –initially to Greek and then to Greek and Latin. It didn’t hurt that I had a girlfriend at the time who’s been my wife now for fifty-seven years. But she was ardent classicist, ardent Greek major at Hunter College. So, I went up when I went off to college after the first year, got into classics and was studying Greek and so forth. And then that got me into Latin, and then I got very interested in a couple of things. One was Hellenistic Judaism. I was very interested in the convergence of Judaism and Greco-Roman civilization and religion. And I had a wonderful teacher at NYU named Frank Peters, who allowed me to explore these things while also sort of directing me towards things that he was interested in. And I, I really thrived with that. Over time, I got more and more interested in science and medicine and the history of those, and I was just thinking about this question. And I pulled down my notes. I was teaching at Hunter in 1974, came back from Stanford, I got my PhD in Stanford and came back and got a job teaching classics at Hunter College. And I was looking at my notes from 1974 and there was like a whole week in my course on Roman civilization devoted to Roman science and Roman medicine, so I already had an interest. You know, when you teach classics, you’re basically teaching military history, maybe literary history. But very few people were at all interested in the classics in the history of science and medicine, and I was very interested. In fact, I had previously taught at the University of California, Irvine. That was my first teaching job and they were very nice and they let me teach a course in Hippocrates. You know, there are five volumes of the writings of… attributed to the founder of Western Medicine, Hippocrates, and I taught that. It was for Greek majors; it was like a third- or fourth-year class. I taught Hippocrates in Greek and Greek science and Roman science. I was getting into that and then somebody when I was working at Hunter, I had a colleague there whose sister worked at… down the block, 68th Street at Memorial Sloan Kettering Cancer Center. She knew that my family, you know, we needed more income than I was making or my wife and I were making at that time. So, she told me about this job opening up as a science writer in the Department of Public Affairs at Memorial Sloan Kettering. And I immediately called my wife. My wife at that time was an editor of a publication called Urology Times. So, she already was a science writer. Some accomplishment. And I suggested that she applied for the job and she said, I’ve got a good job. You should apply for it. So long story short, I applied. That was the same time that I got my Ph.D. So, the Ph.D. was coming in literally like in the mail from Stanford, and they put me to test, they gave me a scientific article to interpret for the public. And I got myself a Stedman’s dictionary and I had my typewriter, and I was sitting at the kitchen table, typing away, trying to interpret all of this medicalese, but it’s all Greek and Latin, you know. All the medical terms are Greek, as you know, are Greek and Latin. So, it was fun because I could use my Greek and Latin in a funny way that I never anticipated, and lo and behold, they hired me. So, I started on June 3rd, 1974. So, I’m coming up on my fiftieth-year anniversary of my time as a science writer, writing almost exclusively about cancer for almost fifty years. Some kind of record, I’m sure, but that’s been my, you know, and I’ll tell you…
Dr. Gary Onik [00:08:31] Yeah.
Dr. Moss [00:08:31] It gets more and more interesting. I mean, I must really have a screw loose somewhere because I was up 4am this morning writing an essay on why you should care about other people’s cancers. How many people do you think there are, you know, worldwide doing something like that? It’s a meaningful question because, you know, we have these forty Moss Reports and they are long, they’re detailed. Each one is, let’s say, about 500 pages in length. I’m sort of curating tens of thousands of pages of writings about cancer that I’ve been doing all these years. But one question that comes up very often, not very often, but sometimes is, well, I have thymic cancer. Why should I care about the person you’re writing, telling me about something that happened with prostate cancer or breast cancer or esophageal cancer? I don’t care about those things or those people. I just want to know about my thymic cancer. So, it raised the… beside for the humanitarian aspect of it, but it raised the question, is it relevant what happens to other people with their cancers? And I would say it’s very relevant. It’s very relevant because first of all, we may not know very much about your particular cancer. So, we have to argue from analogy and doctors do this all the time. Like if you have a cancer of the appendix, it’s rare. So, they’re basically going to treat you like they treat colorectal cancer or sometimes like they treat ovarian cancer or something, you know, because they don’t have enough data really on that particularly rare cancer. But the other reason is because there are commonalities, just like you know, we’re all different, but we’re all the same. I mean, we’re all part of the human race where our bodies are very similar. So, you can focus like modern medicine claims to focus, precision oncology, that sort of thing like we’re going to just deal with you as an individual. But the truth of the matter is that the family of cancer diseases have a lot of things in common. And so, you can exploit those things and you can learn. And the examples I gave in this little essay that I was working on is like the question of blood vessel formation. Like you remember Judah Folkman at Harvard Medical School?
Dr. Gary Onik Sure.
Dr. Moss Judah used to say without a blood supply, the cancer can’t grow any bigger than the tip of a pencil, which is true. So, the formation of blood vessels is a characteristic of—you never say all cancers—but it’s a characteristic of most cancers. So that gave rise to Bevacizumab or Avastin, the first of the drugs to inhibit blood vessel formation. Then there is, there’s now how many did I count? Twelve or eighteen other drugs that FDA has approved to target this so-called VEGF marker of, or facilitator of, new blood vessel formation. Well, it started out, you know, this was going to be a treatment for breast cancer I think, it was the original indication, but it’s now been, there’s now dozens of indications for the anti VEGF or the antiangiogenic drugs. So, this proves that in addition to there being uniqueness to each cancer, there’s a commonality because if the cancer needs new blood vessels in order to grow, to have a class of drugs that inhibit the formation of those blood vessels is quite the same. And if you’ve got a cancer of the thymus, as I used as my relatively rare cancer, it’s still relevant to you. That thymic cancer is still going to need, want and need its blood vessels to get its glucose, keep that speeded up metabolism that cancers have. So, talking about the success of Avastin in treating other cancers is relevant because the odds are very great. We can’t say with a hundred percent assurance, but the odds are very great that you too are going to need a drug like that. If we’re focusing on natural agents, which is my special interest and my special hope that these natural agents would work, then there’s very little cost, either in terms of money or in terms of side effects to taking supplements that affect that, if that’s what your goal is. And so, it is relevant, but you know, these are the kind of things that come up. It’s very good because I get to… I also do some consultations for patients, so I get to hear on the spot what the oncologists are saying and what the concerns of the patient are. And I’ve spoken to thousands of patients, and I think I have a pretty good idea of the lay of the land in terms of what’s really going on, not just reading articles from PubMed, but talking to people as they go through the process and as the oncologists are making their recommendations; very, very, very important.
Dr. Gary Onik [00:14:10] Well, and that’s also where off label use of drugs come in.
Dr. Moss [00:14:15] Yes.
Dr. Gary Onik [00:14:15] You have a drug that works for one thing and you’ve got another cancer and you say, you know what? They’re both vascular cancers. They both have some characteristics that are parallel and so, it’s worthwhile giving that a try. I find that oncology now is so driven by their algorithms that they’re very reluctant to step outside of those cookbook methods that they have right now.
Dr. Moss [00:14:47] Oh, absolutely, I mean, I think if people are not familiar with this, they’d be amazed. You know, the National Comprehensive Cancer Network, NCCN, was formed just 20 years ago by the big three cancer centers at that time, and now it includes, I think, what was the latest figure? Forty-seven cancer centers participate, US centers. So, the US basically gets to dictate to the world how cancer should be treated, and they will assemble the so-called experts on each cancer type. And then they write, what’s acceptable, what’s not acceptable, and we convene every year and see if there’s any need to revise those recommendations. But, you know, this is a consensus document among the so-called leaders of the field. There’s a positive aspect to this in that in some outlying type of places, some doctors were giving treatments that were not necessary, or that were, you know, not justified in the literature. They just were not doing things right. So, I understand, I understand the positive aspect. But the big negative is it homogenized cancer treatment. It used to be if you got a recommendation for one treatment, you could go down the hall and go to a different doctor in the same department and get a different recommendation. Now you could go to China, literally, and you will get the same recommendation or it could be a small list of possible treatments. Most people have no idea that they feel like they’re on a conveyor belt, but they really are on a conveyor belt. I mean, the recommendation is written, and two oncologists have told me in the last year that basically what’s going on is that if you come in with a diagnosis, what actually happens is that that diagnosis gets faxed to your insurance company, and back comes a fax, probably coming from a nurse or a nurse practitioner, maybe a pharmacist saying, here’s the regimen that we’ll pay for, for that stage three thymic cancer. This is it. They looked it up in a book just like everybody else does. They looked it up in NCCN. Or they might say, you’ve got a choice of these two. I’m not saying this is all doctors, but it happens. Two doctors have told me this as I said, in the last year. You go in with your diagnosis, you think you’re getting the wisdom of the doctor. The doctor is just for practical reasons turning to the insurance company, saying basically, well, what do you pay for? What are you willing to pay for? Because they don’t see any point.
Dr. Gary Onik [00:17:42] Yeah.
Dr. Moss [00:17:43] They don’t see, they may think, oh, you know what? That woman who came to me the last time she took those three drugs and she had a fantastic reaction. I’d like to try that again in this patient. It ain’t going to happen, except, you know, in rare, exceptional circumstances because the doctor’s going to have to fight with the insurance company. So, it’s easier to just turn it over to the insurance company and tell us, tell us what you’re going to pay for? Because what’s the point to even discussing this if… and you know, with the cost of drugs like maybe, maybe this is a cancer that will respond to immune checkpoint inhibitor therapy? Well, the cost of Keytruda, to take the most obvious example, is $150,000 a year per patient. One hundred and fifty thousand, surprise surprise, has become sort of the baseline for new cancer drugs per patient. Leonard Saltz at Memorial Sloan Kettering has said that’s parts, no labor. That’s what he said. Parts, no labor. You know, the most effective way to give these immune drugs is to give them in combination. No surprise, they’re also most toxic when you combine Yervoy and Opdivo or Yervoy and Keytruda. Yes, you get a big bump in effectiveness and a big bump in toxicity. So, at the end of the day—and that’s the necessary treatment for melanoma—at the end of the day, he says, it’s more like a million dollars. That’s what’s really going on. So, you may think, oh, I’ve got this patient with, um, you know, with a breast cancer and maybe she has an elevated PD-L1 or tumor mutational burden or something. I’d like to try the immune checkpoints in her. Well, that’s not going to be… may or may not, but it probably won’t be supported, depending on the circumstances by the insurance company. So, you’re going to ask him to pay a million dollars out of pocket to take a treatment? It’s not even practical. So, the oncologist has to do what they can do, and they’re being pressed on all sides. They’re being pressed by NCCN because if you deviate from the guidelines, you are like a lawsuit waiting to happen. How so? Because you ignored the guidelines, you treated how you felt it was the best way to treat, which is how doctors used to, not so long ago, used to treat. And the patient didn’t do well; or, maybe the patient did very well, but then in the end, like most people, the patient dies like most people do, right? Maybe all. Well, as any lawyer would inform the surviving relatives: What? They didn’t treat you by standard medicine, by the guidelines? You know that that person and that man or woman is just asking for it because we could line up ten experts, real experts, people with high credentials and publications and recognized in their field, will line these three or four of these people up, and have them come to court and testify that basically that person is a quack or completely incompetent because we have guidelines for how to treat patients. And they ignored the guidelines and then there’s a multimillion-dollar suit, and maybe disciplinary action following from the state board, and it’s a total mess. And independent practitioners who are going their own way and treating by what how they read the literature and what their clinical experience has been have become very rare. And you’ll notice that a lot of them are older people because younger people are not doing that. Even the naturopaths have basically accommodated themselves to, you know, the standard; trying to soften the edges of the standard treatment.
Dr. Gary Onik [00:21:56] So we’ve already stepped into the realm of the oncology, kind of, industrial complex here. Can you tell us your personal experience?
Dr. Moss [00:22:10] Yeah.
Dr. Gary Onik [00:22:10] I know that you’ve just written a book about it in terms of that and your experience that you personally had at Sloan Kettering.
Dr. Moss [00:22:20] So this was what changed my attitude towards cancer and in some ways towards life. I got that great job at Sloan Kettering, a science writer. And after three years, I was promoted to assistant director of our department, and everything was going very well for me personally. I loved the job. Of course, I still love doing this. I love interpreting science for the layperson. But I ran into a problem, and the problem was, that after a few weeks there, I went up to interview a scientist named Kanematsu Sugiura, who was the oldest member of Sloan Kettering Institute, one of the founding members, and had been in cancer research since the time of World War I. And he was an extraordinary person and extraordinary scientist. When Bristol Myers published a history of cancer research, they put his picture on the cover. So, it gives you some idea of, you know, how he was regarded in the field. He was the scientist’s scientist, and I was interviewing him; sort of nostalgic kind of piece. He was elderly. He was in his eighties. I had just turned thirty. And at the end of the interview, I mean, you know, I was a little inexperienced, I would say as an [inaudible], because I saved for last, like, what are you doing now? I had heard he’s coming into the office, into the lab every day and even Saturdays. What are you working on now? And he said, I’m working on amygdalin. And it took a minute for me to realize that amygdalin was laetrile. We had a book—I was given on my first day of the job, I was given a book called Unproven Methods of Cancer Management, published by the American Cancer Society, and laetrile was first and foremost among, this was, of course popularly known as the quack list. I mean, the treatment, they assembled a list that was sort of like the House un-American Activities Committee, you know, branding every left-of-center group, a communist front. The ACS didn’t want to get left out of the witch hunting atmosphere of those times. So, they had their own witch hunt going on. And laetrile which is an extract of apricot kernels was front and foremost of that, and more and more people were running around the country saying this is a cure for cancer, or the more responsible ones were saying this is helpful for cancer. It shouldn’t be banned; it shouldn’t be attacked. But the position of the National Cancer Institute and the American Cancer Society was very rigid, and it was basically, we know better than you. This is quackery. We tried this. We tested this in in different systems and never worked and has nothing to it. And so, end of story, go away, we don’t want to hear about this, and if you persist in this we’re going to prosecute you for selling quack remedies. There was no internet in those days, but the word could spread very quickly, and it was spreading all over the country. So, I was astonished. I said, Well, what? Why are you working on this if it doesn’t work? And he said, oh, but it does. And he had a uniform lab and very neat, you know, very, very neat. And he had a uniform lab note with that, a little rubber stamp with an outline of a mouse, and he would draw the diameter with calipers. He would get the diameter of the tumor and draw it in on the little stamped in mouse. He had done this so many times that he’d worn out three or four mice stamps. He’d been at this for, you know, for 60 years. Not on laetrile, but on many, many things. You know, he was really extraordinary. And it showed me that when he gave the injection of the laetrile, it would stop the growth of the cancers. It didn’t shrink them, just stopped the growth, and then after a while it stopped working, he said, but that’s nothing. He says what really matters is that it blocks metastasis. And the numbers were—and he showed me all the raw data on this—in the control animals, these were three different mouse models that he worked with, the results were about the same for all of them. But in the control animals, eighty or ninety percent of them had lung metastases. But in the laetrile treated animals, it was only ten to twenty percent. It was as dramatic as dramatic could be. So here was something phenomenal, phenomenal. Of course, it seemed even bigger to me at the time because I didn’t know many treatments, I didn’t know. None of us knew many treatments because this was just, literally, like two or three years after the war on cancer had begun. So not really all that much was yet happening in terms of new drugs or anything. So, I went back, I told my boss about this, he feigned great interest in this. I think he knew over this already. I’ve reason to believe that he knew this. But he said, I want you to keep up the friendship with Dr. Sugiura so that we can know what’s going on. In retrospect, I think he wanted to know what I was thinking about this because now I was in on the secret and, you know, but he said it in a way like, help me, Jerry, understand what’s going on. Sugiura was up in Rye, New York, and we were down in Manhattan, so it was plausible. So, I did. I kept up the friendship, and I liked the man; liked slash loved the man; and I thought this was fine. This is great. Why not? I want to be close in touch with him. What happened next? I’m sorry to be so verbose about this but…
Dr. Gary Onik [00:28:30] No, no, no. This is such an interesting story.
Dr. Moss [00:28:33] Starting in ’74, but going… intensifying in ’75 and ’76, my bosses started to make increasingly negative statements, not just about laetrile—and they’re entitled to their opinion—but about Sugiura and Sugiura’s work. And what they were saying didn’t correspond to what I knew was happening from Sugiura and from other people. Everything that came out of their mouths, actually starting in January of ’74, I would say, was a distortion of the truth. And it culminated in ’76. One of the vice presidents, Chester Stock, told Medical World News we have found a laetrile negative in all the animal systems we have tested. So, this was a complete lie because it was positive in CD8F1; it was positive in AKR leukemia; it was positive in Swiss albino mice. It was positive in all the animal systems that they had tested. So now I knew that there was something screwy here. It was crazy. So, here’s what I did because I couldn’t abide this. I mean, this is not why I got into, you know, writing about. I wanted to write about cures for cancer, you know? I didn’t want to take part in a misstatement about a controversial treatment. I set myself the goal of personally talking to all the leaders of the center. Now I’m nobody. I was, yes, I was in administration, but I literally was like the lowest person other than secretaries. I mean, I was, as I said, I was promoted to assistant director. But I was this low on the totem pole as one normally, you know, one can get. But people liked me. Then they saw me as valuable because I was the publicist. I was the person who was going to write about their… was writing about their work. So, people respected, maybe a little bit feared me because I had an independent mind, obviously. And also, I could help them. I could publicize and publicists, publicity for scientists can be very, very important. So, I set myself this goal. Well, Lewis Thomas was the president of Memorial Sloan Kettering, somebody I admired tremendously at the time for his writing ability and so forth. He won the National Book Award for his book Lives of a Cell and he wouldn’t see me. And he told my boss, Jerry, who didn’t, you know, was not in the habit of lying to me. We were on pretty confidential terms. He said, I’m not going to die on the barricades for laetrile. It’s only a palliative drug. If it were a cure, I might act otherwise, but it’s only a palliative drug. In other words, palliative in the sense that it prevented 80% of the lung metastases in the animals for which it was given. That was… He’s president of Memorial Sloan Kettering. The next one was Chester Stock, vice president of Sloan Kettering, and Chester Stock said when I confronted him with an outright lie, they did a study. It was done by Sugiura’s son in law, and it claimed the study claimed to refute Sugiura because he was unable to get the same results in the same animals. I caught Sugiura and I said, what do you make of this? Now they’re announcing and they want me to write this up. So, I’m doing my due diligence here. They’re saying that they couldn’t reproduce your results and Sugiura said, ask Dr. Stock—that was his big boss at Sloan Kettering—ask Dr. Stock what the dose was that they used. So, first, I called Schmidt. Schmidt said it was the son in law. I said, I want to talk to you about laetrile. He hung up on me. So, then I was really intrigued. I called Stock who is the big boss. I said, Dr. Stock, I’m ready to write this article, press release, or whatever it was. But I do have a couple of questions. Oh, sure, sure, you know, go right ahead. I said first question is what was the dose of the laetrile that you gave to these animals that negated Dr. Sugiura’s work? He said it was 50 mg/kg. I said, but Dr. Stock, Dr Sugiura used 2000 mg/kg. You’re telling me you gave a one fortieth dose of this substance to the mice. That’s right. And you’re telling me that you now have refuted Sugiura’s work with the 2000 mg. He got very angry. He said just write the article; didn’t say damn, but that was the tone. I refused. So I went… we had a big meeting about it next Monday, and I announced at our staff meeting, I refused to do this. I cannot do this. I cannot write an article and say we refuted somebody’s work because you gave a one fortieth dose of the drug. I mean, Gary, how would it be if you know, if you were doing oblation, or you wanted to inject, you know, a drug into a tumor and somebody refuted you by giving one fortieth of the amount of the substance? I mean, it was that blatant.
Dr. Gary Onik [00:34:36] This is the portion of the podcast where we talk about advances in cancer that should give our patients hope. Today, I’d like to bring to our listeners’ attention a new advance in metastatic prostate cancer, particularly castrate resistant metastatic prostate cancer. Castrate resistant metastatic prostate cancer means that the main way of treating metastatic prostate cancer, which is to chemically castrate men, does not work anymore. So, they become “castrate resistant.” Once a patient becomes castrate resistant death is sure to follow rather quickly. There is, however, a new, very promising treatment for castrate resistant prostate cancer patients. And that is PSMA, linked Lutetium-177, which is a radiation source that is a very focal radiation source. It emits radiation that goes only a short microscopic distance. Now the key to this treatment is that prostate cancer makes prostate-specific membrane antigen that can hook to another molecule that we manufacture that binds to it. And that molecule is hooked to the radiation. So, what happens is we give this PSMA molecule that’s hooked to Lutetium-177 to the patient, and it goes and finds the PSMA in the patient’s cancer cells and delivers radiation almost specifically to each cancer cell. Very clever. And I’m sure we’ll have many implications for other cancers when we find particular molecules that will bind to other cancers. But now we have a very specific and actually very safe radiation for prostate cancer patients at the end stage of their disease. This has been shown to, in a large study, to improve survival in metastatic prostate cancer patients who are castrate resistant. At this point, it’s only an increase of four months. But that’s quite remarkable when you think that it’s only the first study, and we have to find all of the ways that we can optimize those results. So, I think that this is a great day for metastatic prostate cancer patients who are castrate resistant, and it should give all of us who have had prostate cancer some real hope.
Dr. Gary Onik [00:37:53] This is the segment of the podcast that we call the mailbag. Our listeners get to send in questions for me to answer. We don’t answer questions that deal with specific medical problems for a specific patient. There’s no possible way we can answer those properly and so those go to your oncologist and your physician to answer. Ours are more general in terms of how to deal with cancer and those types of issues. So, we have a question sent in by Jane in Florida and it says “I’ve been diagnosed with terminal cancer. I don’t want to tell my children who live in other states or my ex-husband about my diagnosis. I don’t want to be a burden to them. Am I doing the right thing?” Interesting question. And I’ll give you a very straightforward answer. No, you’re not doing the right thing. It’s not the right thing for you, and it’s certainly not the right thing for them either. And why is that? Well, the first thing is we had a guest on our podcast, Karen Schueler, who wrote a book called The Sudden Caregiver. And that book really was about her experience of taking care of her husband, who was diagnosed with terminal cancer. And one of the most seminal moments and most important concepts to come out of that book is that the caregiver actually experiences something positive, which she calls a grace, and that it is a very positive experience for the caregiver and subsequently that obviously reflects on to the person getting the care as well. So, by not telling your children, you are, in a sense, depriving them of what could be a very positive experience and certainly depriving yourself of a tremendous amount of support that you’re going to need through this process. I know that when I was diagnosed with cancer, and I didn’t ask my daughter to come down and take care of me when I was being treated for it, and you know, she’s still pissed off at me about that. I mean, she wanted to be there. And she’s pissed off that I didn’t allow her to fulfill, you know, one of the roles that she felt that she should fulfill as a daughter. So, I learned that one the hard way. What about your ex-husband? Well, that’s really a tough one, because I have no idea what your relationship is with your ex-husband. But let me give you an example in my world, when I was diagnosed, I had an ex-girlfriend who when she found out about my diagnosis and I was going to have some uncomfortable treatments and I was going to need some care she stepped right up and took care of me when she really had no obligation to in terms of our situation. And I will thank her for that forever, for stepping up at that time that, you know, I really needed her. So, you know, depending on what your relationship with your ex-husband is, you might want to tell him because you might be surprised at how much positive aspects he can give to the situation.
Dr. Gary Onik [00:42:04] If you would like to ask us a question for the mailbag, you can go to garyonikmd.com. There is a contact form that you can fill out that will be forwarded to us, and we’ll consider your question for our show. Thank you for listening to our podcast. I hope that it provided you with some useful information, some hope and some comfort. Thank you very much.