View this episode's trailer
Episode Description
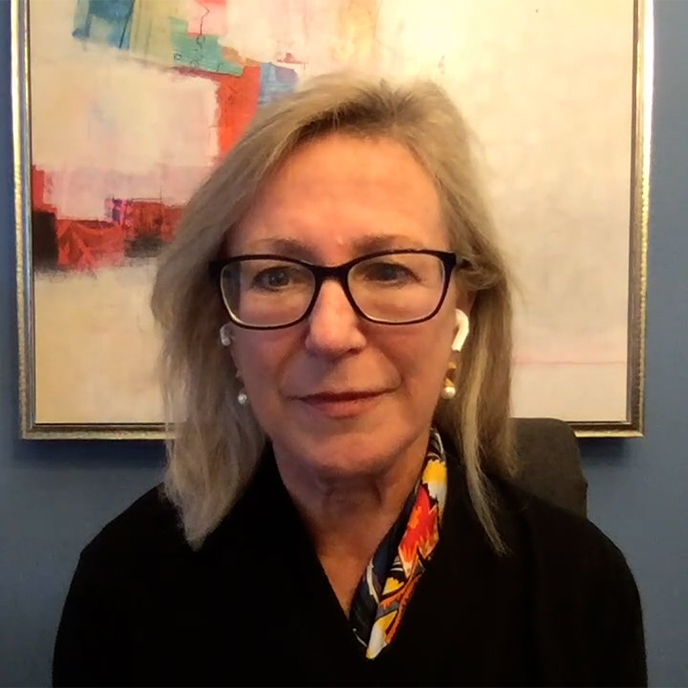
There are 53 million caregivers in the United States, probably a lot more. If you know one or should you suddenly find yourself as one, you need to hear Dr. Onik’s conversation with Karen Warner Schueler, author of the transformative book “The Sudden Caregiver: A Roadmap for Resilient Caregiving.” This is also a conversation for medical professionals, especially in the oncology field. Her book is filled with ideas, encouragement, and resources so you can also take care of you. After all, the better the caregiver, the better the care receiver.
After raising a family and reaching a comfortable stage of life, looking forward to their future together, Karen’s husband went to his doctor for a ‘bad back’ and came out with a stage 4 cancer diagnosis. Thrust into the role of caregiver, depleted and vulnerable, she found resources lacking. So, she wrote the book she wanted to read—to help caregivers write their own story.
Learn from Karen…
- The Paradox of Caregiving
- Where to find REAL hope
- The Pathways to Wellbeing
- Who needs to work at empathy
FIND links to organizations that provide local, national, and international caregiver support under the “Resources” tab on her website http://thesuddencaregiver.com.
For over 40 years Dr. Gary Onik has been pioneering advances in cancer treatment that have rocked the field of oncology, inventing an entirely new branch of cancer treatment now known as “Interventional Oncology” based on his innovative minimally invasive techniques. Both doctor and patient, he created a cancer vaccine and successfully treated his own terminal prostate cancer using his invention. In addition to his medical practice, Dr. Onik is an Adjunct Professor of Mechanical Engineering at Carnegie Mellon University, working closely with his colleagues to develop the next generation of cancer fighting technologies. His latest work, using immunotherapy to treat metastatic cancer, offers hope to those patients with literally no other options.
TO CONTACT DR. ONIK visit https://www.garyonik.com/.
TRANSCRIPT
Dr. Gary Onik [00:00:00] Hello, I’m Dr. Gary Onik, and I’m your host for Cancer is Tough, but YOU are TOUGHER! I want to thank The Beach Boys for allowing us to use their piece of music that is dear to my heart. My podcast is uniquely personal. I know both sides of the cancer equation. I am a cancer specialist and researcher, as well as a cancer patient and survivor. I will address various treatment modalities in the podcast, but that’s not really what this podcast is about. This podcast is about the unique cancer journey that a patient and their family and friends take when they are diagnosed and treated with this dread disease. We’ll delve into the inner emotional and spiritual resources. Patients and their loved ones need to address their concerns of choosing a treatment strategy that will harmonize with their worldview while grappling with state-of-the-art treatments versus alternative treatments. When I was asked who’s going to be my target audience, the obvious answer was everyone. It’s a rare person that has not had cancer touch their lives, either as a patient, a family member or friend. If you’re that rare person that hasn’t had cancer touch their lives, almost certainly at some point, cancer will drag you into its maelstrom. I hope that you find this show both a resource and a comfort in dealing with your cancer journey.
Dr. Gary Onik [00:02:21] We have with us today, I think, a very special author. It’s Karen Warner Schueler. She has written a book called The Sudden Caregiver A Roadmap for Resilient Caregiving. I think, Karen, that this is really a transformative book. I put it in the category of Jordan Peterson’s 12 Rules for Life.
Karen [00:02:48] Wow.
Dr. Gary Onik [00:02:50] No, I’m serious. I’m really, I’m really serious. Well, tell us a little bit about the statistics of caregiving and why I’m saying that.
Karen [00:02:59] Well, there’s 53 million caregivers in the US, I actually think there are a lot more. Caregivers are… make up 11 percent of the populations of the developed countries. And one reason why I decided to write my book is when I became a caregiver, I wanted a manual that would tell me how to be the best caregiver. There is research that says the care receiver, the patient in your care, the person in your care will have a better experience in their own medical situation if the caregiver… the better the caregiver is, the better the care receiver is. And when I realized that, I was sure that I was going to blow it unless I found something, It’s literally a matter of life and death. So, right. So.
Dr. Gary Onik [00:03:54] I mean, there isn’t a bigger thing to blow really. So, you might as well go all the way.
Karen [00:04:01] Very true.
Dr. Gary Onik [00:04:03] I want to read a quote here from the… basically the book jacket. “The Sudden Caregiver shines a light on the paradox of caregiving—that caregiving offers moments of both grit and grace. This book will change the way caregivers give care, and it might just change the caregivers’ story for millions around the globe. If you’re a caregiver, you need this book, and so does the world.” Now there are five other just as laudatory quotes. I’m in the middle of book. I have to tell you I’ve read two thirds of it. I’m going to finish it. There’s no question about that. And I agree wholeheartedly with this. There are going to be a stack of those books in my waiting room, and I’d like to return to this in, you know, a little bit later because I think there are some implications that I’ve seen in reading all of those, that I want to talk to you about.
Karen [00:04:56] Great.
Dr. Gary Onik [00:04:57] With that said, let’s return back to your story. Tell us a little bit about your life and your relationship, you know, with your husband before the big explosion or catastrophe or give it other names. But it’s changed your world. Tell us a little bit about that, please.
Karen [00:05:23] Well, the day before I became a sudden caregiver, it was business as usual, life as usual. My husband and I had, we each have, we’re a second marriage, so we each had grown children. They were launched. They had partners. They had jobs. Everything seemed great. In June of 2014, which is when we got the diagnosis, my husband and I went to Rome and went to Italy and for the first carefree vacation we had ever had. And we had that feeling of, we made it. We did it, and life will now blossom and unfold for us. We’re both consultants. He, we used to say, he was the big planet, I was the little planet. I’m an executive coach. I take people wherever they are on the ground and help them grow and get out of their own way. He was already a big guy in the world. He has a big footprint. He worried about things like carbon footprint and global economy. He wrote and created with PricewaterhouseCoopers in the Carter Center, something called the Opacity Index, which literally measures corruption, opacity, transparency in 54 countries around the world. That’s how he thought, and I was the person who said, we should go to Italy for a vacation. What do you think? So that was our world. We had many conversations before that trip to Italy, where we were trying to hit reset, like, who do we want to be? I had a business that kept me traveling on the road, frequently going to my clients’ sites. He was going to Dubai and traveling all over the world, and we were trying to figure out in that summer how do we come together? Our daughter was getting married in October of 2014. And that was where we were. Life was open and it was a fast car in an open road, and in Italy, which was June, there was no sign of cancer, but within three months he had been diagnosed with stage four cancer. I would say he was diagnosed with lung cancer and I would say there were no symptoms of lung cancer. But all summer after that trip to Rome, he kept complaining about a bad back. And when he finally, I was on the road with a client doing a leadership class, and he called me on my break and he said, I’m in a lot of pain. So, I called a friend, our best friend, and got him to the hospital and when I finished my day, and I was sort of like, do I just go home? It’s probably no big deal. He’s going to be… so I just kept waiting for the call. I come home from the E.R, they did an MRI, I have a bad back. And when I fell asleep, fully dressed, waiting for that call and at two o’clock in the morning, the call came and he said, I have stage four cancer, and it was so unreal to us that we just joked about it. And for me, I thought, OK, I’ll catch the next flight, I’ll get to the hospital, I’ll talk to them and I’ll show them that they’re incorrect. That this is not possibly a stage four cancer diagnosis. And I stayed that way for about seven days. And then the reality really began to kick in. And then you shift to, OK. So overnight I’ve become a caregiver. How do I do this as well as I can?
Dr. Gary Onik [00:08:53] When I was diagnosed with terminal prostate cancer, when I found out, it’s hard to describe, but everything… I can remember everything about it. I can remember where I was. I can remember the actual feelings that I got when that happened. And so, I can relate a little bit, you know, to what you’re saying. This first portion you’re describing and I had this to write, I wrote this down because I… as one of the questions I wanted to ask you. You, it’s you’re almost like, you’re following Kubler-Ross’s five stages of death and dying. And one of the things I want to say was… is that, is Kubler-Ross passé and not relevant anymore? Or as you are describing this, it sounds like and you’re very conversant in these things. Did you see this happening along those lines?
Karen [00:09:53] Yes, I mean, that was always in my mind, but I also felt like I went through those five stages like within an hour or within a day. So, you’re in denial, then when you get to acceptance, I got it. It’s on me. I’ve got to do something. So that was always in the back of my mind. I would say my lived experience was a little more abstract than that, just trying to do whatever was required in the moment. But if I sit back and reflect on it, I would definitely say that’s relevant.
Dr. Gary Onik [00:10:24] I mean, it’s interesting because I did exactly the same thing as you. I was alone at the time, so I needed to get through it, and I went through the five stages. An hour later, I was at acceptance and I had to show that I made up T-shirts that said, you know, Yeah, fuck Kubler-Ross, I’m going to send you one of those, OK?
Karen [00:10:50] Absolutely.
Dr. Gary Onik [00:10:53] You know your book talks about the caregiver’s paradox. Can you explain to me what that is and our audience what that is? And how it’s really one of the kernels of what you’re talking about.
Karen [00:11:09] Thank you so much. I feel like for your listeners, this is one of the most important concepts of my book, and I almost didn’t recognize it. So, what was happening was when I am a reader and I am someone who turns to books and research studies to find out what my experience should be. And when I turn to research, well-founded gold standard research, what I was seeing was, man, if you’re a caregiver, you’re more susceptible to the disease than the person in your care. You’re more susceptible to mortality than the person in your care. After that person resolves whatever their situation is, you’re screwed. And that during the situation, you’re going to be depleted, you’re going to be out of energy, you’re going to be afraid, you’re going to be worried about finances, you’re going to be worried about running out of time. Those things, which is what the research said would be my experience were absolutely my experience, and they were not the only thing I was experiencing. And so, one day when I was doing my, you know, how do I be a better caregiver research I stumbled upon, there’s a thick report from the Forum on Aging, and there was a graphic in it, and there was a study representing a study that had happened where people talked to caregivers and they asked them, this graphic’s in my book, but they ask them to rate a series of experiences. Five of them were negative, like, do you have enough money? Do you, are you doing a good job? And three of them were positive. Do you feel like you’re closer to the person in your care? Do you feel like you’re adequate to the job of caregiving? And what I noticed was just in the scores that all the stuff that’s depleting and negative was sort of like in the forty-eight to fifty-three percent of significance to a caregiver. But the things that were positive were rated at the 90 percent level and that gave me pause. And it was just one study, but I decided I would start, just people were reaching out to me as caregivers to ask for my help. And so, I just started asking them, what is your experience? And what I heard is, I talk about it briefly in my book. It’s a concept that comes out of the University of Pennsylvania. Martin Seligman. I have a degree and master’s in positive psychology from there, it’s the mothership, and it’s a concept called Perma. And what Perma is, is there are five elements that are probably present if you’re in a state of well-being, positive emotions, engagement, positive relationships, meaning and accomplishment. And when I listen to what caregivers were saying to me and what my own experience was, I would say, hi Perma. And so, caregivers would say, one person said, this is my, I’m not an artist, I’m not a singer, I’m not talented specifically, but my parents need me to be their best caregiver, and this is what I’m put on Earth to do. That’s meaning, that idea that this is my purpose in life and I can tell you story after story, including my own where that’s true so that the caregiver’s paradox is, it is both depleting, it is absolutely on any day of the week can be, I can’t do this, this is still going on. I can’t do it one more day, and it’s a source of well-being.
Dr. Gary Onik [00:14:43] It’s anti-intuitive in a way, isn’t it?
Karen [00:14:46] Yeah. Yes, it is.
Dr. Gary Onik [00:14:48] But it’s very uplifting. Talk about hope.
Karen [00:14:52] I know that you are called Dr. Hope sometimes, and that is what the purpose of my book is, is to provide a different story that you can write for yourself and a story of hope. So, in my world view, and I don’t know, I’m lucky, I think I was just born this way because there’s no reason to think that I earned this. But in my worldview, it’s never… until you, unless you’re talking about terminal cancer, there’s not a problem you can…
Dr. Gary Onik Yeah.
Karen And you can apply if you can figure out a way in. And if you hit a wall, there’s… you’ll climb over it, go around it, there’s a way. And that is constitutionally how I approach everything in life. So, when I thought about that, I thought, is it possible to cultivate that? And here I am talking to caregivers who are telling me they have well-being and that’s not what was being researched and documented. So, I thought, well, if we intentionally create a state of well-being, if we intentionally in every moment go, oh, I can’t do this one more minute and well, you know, what am I grateful for in this moment? What is good and what is happening, if we have that ability to reframe, to look at it through a different lens? And we are humans, that’s the only renewable ability we have, is to take out of a situation what will serve us, if we, as a caregiver I can tell you, you wake up and go. I don’t feel like being resilient today. I don’t feel like being happy. This gratitude, uh I have to write in my gratitude journal.
Dr. Gary Onik [00:16:37] You’re just, you’re describing me in the morning, right? I’m not a morning person.
Karen [00:16:43] You’re driving, the windows are closed and you’re screaming about, why cancer? Why now? Why is this happening? I mean that, that’s all-true stuff, but it’s not the only thing and I… So, there’s two parts of my book, one is the pathways to well-being and that’s really six things I came up with, based on evidence out of positive psychology and other areas where it’s possible to create your own resilience, your own world where you can filter some of the things that go on. The other part is a road map, because not only do you have to be a certain way as a caregiver, you have to know what to do. And those were the two things. But in terms of hope, and I talk about this a little bit in pathways to well-being, hope is not, ok I’m going to be Pollyanna, I’m going to hope that this cancer diagnosis isn’t true and we’re going to get, we’re going to go into treatment and we’re going to have an experimental clinical trial and boom. It’s… the tumors go away and we’re back to booking our trip, our next big vacation. That’s the big hope. And if someone had told me, what are you hoping for, that would have been it. But there’s some work by Chris Faulkner out of University of Pennsylvania Hospital, and he talks about, ok, what are the things we can hope for that are rational, reasonable things? So, I could hope for, we have all our relatives, our family, over for the holidays and it’s the best time and however many more holidays we have, that’s how we’re going to do it. So, I could hope for that. And that’s a hope I could deliver on.
Dr. Gary Onik [00:18:26] That’s a wonderful, wonderful way to put it. I mean, you know, my job is hope. The first great hope is, yes, I’m going to, you know, do something miraculous and cure you. But if that doesn’t happen, you know, then there are those lesser hopes. Yes, we can, we can work with you and give you, you know, perhaps more time, but good time, you know, not you’re sick all the time and your hair falls out and you know, you don’t want to be living through that time, but good time. And then it, then it comes down to the next level, you know, hope that we can, we can put you there, you know, to where you want to be without any pain. And then finally, that we can help you accept, what the, you know, what the end is going to be, so I completely agree with your approach to hope because most people do think about it as, I hope we can, you know, get into the trial and sometimes that happens. I mean…
Karen [00:19:26] I’ve been before, that that’s happened to absolutely.
Dr. Gary Onik [00:19:29] Well, I personally know it. So, you know, I mean, there are some listeners that may know my story, but that’s not germane to what we’re talking about now. The, one of the cogs in this one of the pillars COGS, there are 10 different ways you can say, but one of the most important entities in this is the medical profession, ok. Your oncologist. I’d like to know what your experience was with oncology, traditional, you know, you traditionally. Did you feel that it served you completely well? Were there things that you felt were inadequate there? I’ve got my own feelings about that because I’m dealing with oncologists all the time.
Karen [00:20:09] I think on our oncology team was a part of the overall puzzle, and I think for your listeners, the one thing that was an aha moment for me about a month into our crisis, our diagnosis, was we’re incredibly lucky because of where… my husband was a fellow at the Milken Institute. Mike Milken, you may know Gibbs. He’s a very philanthropic, very philanthropic when it comes to especially pancreatic cancer, but other cancers. He was so helpful in just putting us in the right place. We were in Boston and we ended up at Dana-Farber, and Pasi Jänne was, because it was lung cancer, he’s a thoracic oncologist. In the beginning, the oncology team was very… they were, I wouldn’t say they were pie in the sky, it’s all going to be fine. But they did say in a very helpful way, it’s too soon to tell what your trajectory is. We… you know, they said that in the first visit and they were terrific when it came to what they’re supposed to be terrific at. Well, as a caregiver, I thought, I’m going to walk into Dana-Farber Cancer Institute, the greatest cancer institute on the planet, and we are so lucky to be here. So, they’re going to put an iPad in my hands and it’s going to be, you know, I’ll just put in what kind of cancer we’re dealing with, and they’re going to tell me what to do. And what I was looking for was, what about alternative therapies, not just chemo? What about diet and nutrition? What about integrative therapies? What about acupuncture, meditation and I would ask them and they were kind of noncommittal, like, well, some people have had success. Because they’re not… that wasn’t their job and that was my moment of saying I keep petitioning these people to tell me basically how to make in-between chemo good for my husband.
Dr. Gary Onik [00:22:18] I don’t… But you’re cutting them so much slack there. Of course, it’s their job. That’s part of their job, don’t you think?
Karen [00:22:25] I didn’t think so. I really…
Dr. Gary Onik [00:22:28] Okay. That’s fair.
Karen [00:22:29] Yeah. Well, at least that was my realization that they’re curing cancer. That, I mean, Dana Farber, that is the goal. Let’s find a cure, let’s find… Meanwhile, we’re going to treat these people who have cancer. I mean, that’s the… that is the teaching hospital. That’s what they were about. So no, I felt like they did their jobs. If I had any criticism at all, it’s that when it came to the end… And I, actually, this is not limited to our oncology team, this is the medical profession in general. I think they have to work at empathy a little. And so, my job as caregiver was to make us real and human so that they would see us as people and not just patient. And this person who’s coming in with this patient all the time who happens to be a caregiver. I feel like they are behind steel doors like they see death in front of them all the time, and we might be that. So, there’s a bit of a distance and I felt like my job was to grab those steel doors and keep them open and show them who we were. And I feel like we did that pretty well. I think that the other piece of information, it’s not a criticism, it’s just this is how I’ve experienced it is. They already know all the way to the end what’s going to happen. So, when the cancer moved to my husband’s brain, they told me in a way, I wrote it down, he might have three months to live. But he… no one said those words. It was just, well, this will run, of course, and we’ll check in in three months and then I’d go home and two days later go, oh, they’re telling me… So, there is a part of caregiving, if you’re supporting someone who’s in medical care to really go that extra mile. So, I felt like they’re giving me all but the last piece of information that they’re holding onto, and if I could pry their hand open I would find out we have three months here; we have to make the most of it. And I don’t envy doctors because you can’t sit someone down and go, ok, this is about 18 months here and you have to just, they let the rope out a little bit at a time. And as a caregiver I just, just tell me I just would rather know.
Dr. Gary Onik [00:24:55] No, I understand. By the way, I did do my first fellowship at Dana-Farber, where we developed the first new treatment for liver cancer. So, I’ve been part of that world and I know what that’s like. There’s actually a time in my career when I was so affected by patients that it was affecting my judgment. Where I actually had to bring myself away from it and because I was doing experimental things and I was trying to do things that were impossible and patients were suffering because of me having sometimes too much empathy for their situation.
Karen [00:25:34] Yeah. Wow.
Dr. Gary Onik [00:25:35] So now, you know, I can… I can really, I can relate to that. This is a nice point for me to talk about. You know, when I was looking at those quotes and they’re all, they’re all true and they’re all highly laudatory. But the thing I noticed was that there was not a single doctor or oncologist there. And I just want to know, because if this is going to really have the impact that it needs, we have to get the oncology world into this. So, they see this as an important part of their job. I mean, if you just told me that the people that were, you know, that were helping you with the college were not part of that, in a sense. So, you know, this is a blind spot. Do you have any plan or do we have to come up with one to get this in front of the oncology people?
Karen [00:26:33] So the reason that I don’t have those are… there’s kind of two reasons. One is kind of the way I’m wired because when I was seeking those, those quotes, those laudatory quotes, it was at the height of COVID. And the people that I know who are in the medical profession were kind of fighting for their own lives and sort of protecting themselves. And the way I’m wired is, ooh, I don’t want to ask. This is such a small thing. I mean, it wasn’t even a book yet, it was a word doc. And I don’t want to ever impose myself or and that is just… I’m a Girl Scout, polite kind of person. So, Pasi Jänne, did, he received the book and he and I had spoken about the book when my husband died, and he sent me a note when he received it, but the book was already out. But he said, Dear Karen, thank you so much for sending me your book. I remember you telling me you were going to do it, and it’s amazing to see the final product. I’m sure many families and caregivers who are faced with the cancer diagnosis will benefit from your book and the strategies you lay out. I hope you’re doing well and staying well during this pandemic. But when I got that, I was like, whew…
Dr. Gary Onik [00:27:51] It was lovely. Yeah.
Karen [00:27:53] Yeah, yeah. And just didn’t have to do it at all. But one thing that I would love is now that the book is a book, it’s been so well-received by caregivers, by… I just recently had some surgery and gave a copy of my book so that I would get inside the steel doors, get some empathy. I gave a copy of my book to my surgeon and he, because it has the word resilience on it, we ended up having a very serious conversation about resilience in the medical profession because it’s so challenging right now. So, that’s my answer. I didn’t want to impose upon doctors, but I agree if I could get this into every waiting room in the world… No, seriously. I thought, Well…
Dr. Gary Onik [00:28:42] That’s… we got to figure out a way to do it, because it’s where it’s going to have its greatest impact.
Karen [00:28:47] I agree.
Dr. Gary Onik [00:28:48] I’ve got one last question. You’ve been so gracious giving me your time. My last question is you seem to be someone with some aspect of spirituality not talking about religion or… it could be religion, but you seem to have this feeling of spirituality about you and about the process you’ve been through. Am I right or where is that in how you see your world view and what you’re doing now?
Karen [00:29:20] It is correct. I was raised Roman Catholic in Philadelphia, went to parochial school, and that is culturally a lot, a lot about who I am. It was a good experience for me. But when I was going through caregiving… I’m a person, even without caregiving and without crisis, where I’ll just on a regular basis say, ok God, do you see what’s happening here? And it could be like I’m doing a home improvement project, and it’s… or I just want to, you know, want to reach out to my daughter but she’s busy and I can’t get her on the phone. So, I’m a person who both asks for help spiritually and also thanks. And I perform little acts of gratitude that when I feel like a prayer has been answered, I don’t consider myself particularly religious, but I do believe there has to be something bigger than us. There’s a chapter I wrote that didn’t make it into the book, but I’ll share it with you on this idea of spirituality, which is that I do think that, I think that Joel, my husband, my late husband, is kind of around. Especially after he passed away in that very first year of grieving, the problems I had were huge and intractable, and I would be walking the dog and I would find a little stone shaped like a heart and take it as a message. And that was something wherever we traveled we would always, like, if we took hikes we’d find heart shaped stones; they’re everywhere, by the way. And so, I would feel like, I would get a little, like, it’s going to be ok message laid into my path sometime, you know? Is that a rational thing to think? I believe so. It comes from someplace outside me.
Dr. Gary Onik [00:31:14] Well, let me tell you a story which relates to this, and it’s so germane to what you’re saying. I had a patient. He and his wife had this wonderful relationship very much like your husband and you did, and they were just like one. And he did well for a while and then finally passed away. And when I called her to talk to her about, you know, how things were going with her, you know, now that he passed away, she said it’s, you know, it’s very… it’s very good now. And she told me the story of three days after he passed away, she woke up in bed and she couldn’t see him, but he was there in front of her. And she said he let me know that we would be together again. He let me know that everything was going to be all right. And she said it changed you know, her whole world after that. And it sounds a little bit like what you’re basically describing.
Karen [00:32:25] Yeah. Yeah. I had a very similar experience, and that’s the part I didn’t put in the book, but maybe it did make it. I can’t remember. It seemed a little out there, so I was on the fence about including it. But there were a lot of things entwined that when my husband passed away, I found out he hadn’t really settled, partly because I think he just thought he’d have more time before he lost his ability to sort of… he was the master of the universe, and he was no longer master of the universe. But I don’t think he meant to do it to me. But my sister on my birthday said, you know, I got this message. She talked to a channeler and the message was that he came through and said, tell Karen I’m sorry, I ran out of time. And then there were financial things, there were real estate things, there were things that I didn’t feel equipped and was surprised that I had to deal with. And after, we had just finally sold our family house and I came home and got in bed and, you know… I had my bed, I still kept the whole bed like half of it was made because that was his side and I would just slip in the covers. And I woke up and he was there lying beside me, and he was wearing his Berkeley T-shirt and his jeans and, you know, he opened his arms up and I went, you know, laid against him. And we just talked, and we talked about the kids and the grandchildren and all the things that were part of the future that he didn’t get to see. And in that, he said to me, it’s going to be fine. I know you’re really scared, but it’s going to be fine. And he said you seem really tired. And I said, I’m afraid to fall asleep because when I wake up, you’ll be gone. And he said, I’ll stay. And I fell asleep, and when I woke up, I looked and he was there and it was this dream was literally, this is my bed. That’s the window, here he is. And then I fell back asleep, and when I woke up, I had the sense of just peace. And that is what stayed with me. That idea… he was the person who protected all of us and made it all. If any of us had a problem, he was just a great problem solver and so… I share that with you.
Dr. Gary Onik [00:34:56] So, Karen, can you tell us what, well, tell us about your website and then tell us about the resources that we’ll find on there to help us with being good caregivers?
Karen [00:35:08] Well, thank you. My website is thesuddencaregiver.com. And one thing that I learned as a caregiver is that I was using my own resources. Caregivers typically spend about $5,000 out of pocket a year that will never be covered by medical insurance. And I realize that there are organizations local in our community and also national and international that are there to support caregivers. So, on my website, there’s a tab called Resources, and if you click on it, there are tiles that are the logos of various resources that might be supportive to you as a caregiver. One of the things that I worry the most about that I couldn’t solve writing my book is the lack of resources that some caregivers face. That $5,000 out of pocket. Where are people going to get that? Especially if your work life is compromised, you can’t work as many hours; you may lose your job. These are all things that happen to caregivers or the medical state of the person in your care means you can’t afford to bring help in, but you can’t leave the house in order to work. So, there is a resources tab on the website where caregivers might find some support, some extra formal support. Social support.
Dr. Gary Onik [00:36:34] Thank you so much. I hope we get to talk again because we’ve just scratched the surface on some of these things that have so many implications. All I can do is thank you for your extraordinary contribution and for this teeny-weeny contribution to us.
Karen [00:36:54] Thank you so much for inviting me to be part of your show for the work that you do, with the people that you reach, with the ideas that they have to… it would just lighten their load and I really appreciate that you’re doing this.
Dr. Gary Onik [00:37:10] Thank you.
Dr. Gary Onik [00:37:26] This is a segment of the podcast where we discuss the hopeful trends in oncology and cancer research. Today’s topic is going to be about the FDA. I know that the FDA at times is looked upon as a villain in the cancer world, and I honestly have to tell you, I found that that is not the case in any way, shape, or form. I’ve dealt with the FDA in my own experience, and particularly the oncology segment of the FDA really bends over backwards to try and get treatments out there for patients as quickly as possible. There’s even a program called the Breakthrough Designation, where a certain treatment that looks like it is a breakthrough that treats a cancer that has no good options, accelerates its approval. The FDA works with the investigators and the company to make sure that the study is being done properly and that when the results come in, the study can be approved in most expeditious manner. So, I think that this is probably one of the most hopeful things I can say, is that the government is not getting in your way to have the access to treatments as quickly as possible.
Dr. Gary Onik [00:39:22] Well, welcome to the segment of our show where we reach into our mailbag to answer questions from our listeners. The parameters that I want to give you since we’re early in our podcast experience is that I really can’t answer a personal question about your specific problem because there’s no way that I can have the background of your history to answer specific medical questions for you. We’re going to deal more with the general aspects of oncology and perhaps spiritual things, practical matters that you’d like to know about and the approach that you might want to take to your treatment. So, with that said, let’s get going and read our first question. This is Bob from San Francisco. “My uncle was just diagnosed with pancreatic cancer. How do I know he is choosing the right oncologist for him?” OK, this is an interesting question, because it has a number of points of view and some of them are actually opposed to each other. The first point is that it’s a dire diagnosis. You really want to be at an institution that has as many advanced options to treatment as possible, that does clinical trials and can get you into clinical trials that may offer you some more hope than you might get out in the community. That’s the first aspect. The second aspect is that it is a dire diagnosis, and it’s critical that you have an oncologist that can really guide you through the process and that you feel really comfortable with, who will be there for you when hopefully good things happen. But with this diagnosis the more likely is that the bad things are going to happen and you really want somebody that you can depend on to be there. I know as a doctor, I try and call the major medical centers all the time about some of my patients to speak to their other physician, and I can’t even get through to them. Let alone having a patient try and get through to them. So, you know, I think that maybe a combination of both, that you have a local oncologist who can help you. Most oncologists will be able to go on clinicaltrials.gov and find out any trials that might be open for you or your relative. And so, I think a combination may be the best approach. I also think there’s another aspect, and that is that, you know, I believe that our consciousnesses interact with each other and that there’s no question that if you are compatible and it makes you and your oncologist gives you a positive feeling that that is going to have an effect on how well you do. So, you know, add that into the mix. And, you know, I think that at least have some guidelines as to how to go about it.
Dr. Gary Onik [00:43:14] If you would like to ask us a question for the mailbag, you can go to garyonikmd.com. There is a contact form that you can fill out that will be forwarded to us, and we’ll consider your question for our show. Thank you for listening to our podcast. I hope that it provided you with some useful information, some hope and some comfort. Thank you very much.