View this episode's trailer
Episode Description
"I haven’t had a sick day since I was diagnosed."
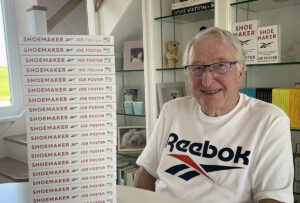
Dr. Howard Freedman is a retired pediatric ophthalmologist renowned for inventing a way to screen children as young as 6 months for amblyopia, lazy eye, one of the most prevalent—yet preventable—causes of blindness in children.
He’s also been diagnosed with cancer, twice.
In this episode he talks about the obstacles he faced while trying to make inroads within the medical community to help kids who would otherwise unnecessarily lose their vision, a true healthcare tragedy. And he shares his cancer story. Two journeys, one professional and the other personal, have surprising parallels.
These two physicians share important REVELATIONS in:
- The forces that try to stop therapeutics that really help people.
- The basic problem with medicine when trying to change the status quo.
- Seeking multiple opinions and exploring those with a doctor you trust.
- Choosing treatments that allow for a normal lifestyle.
Dr. Onik shares his Medical Golden Rule perhaps the single greatest factor owing to his incredible success.
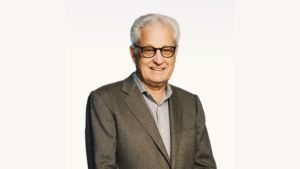
For over 40 years Dr. Gary Onik has been pioneering advances in cancer treatment that have rocked the field of oncology, inventing an entirely new branch of cancer treatment now known as “Interventional Oncology” based on his innovative minimally invasive techniques. Both doctor and patient, he created a cancer vaccine and successfully treated his own terminal prostate cancer using his invention. In addition to his medical practice, Dr. Onik is an Adjunct Professor of Mechanical Engineering at Carnegie Mellon University, working closely with his colleagues to develop the next generation of cancer fighting technologies. His latest work, using immunotherapy to treat metastatic cancer, offers hope to those patients with literally no other options.
TO CONTACT DR. ONIK visit https://www.garyonik.com/.
TRANSCRIPT
Dr. Gary Onik [00:00:00] Hello, I’m Dr. Gary Onik, and I’m your host for Cancer is Tough, but YOU are TOUGHER! I want to thank The Beach Boys for allowing us to use their piece of music that is dear to my heart. My podcast is uniquely personal. I know both sides of the cancer equation. I am a cancer specialist and researcher, as well as a cancer patient and survivor. I will address various treatment modalities in the podcast, but that’s not really what this podcast is about. This podcast is about the unique cancer journey that a patient and their family and friends take when they are diagnosed and treated with this dread disease. We’ll delve into the inner emotional and spiritual resources. Patients and their loved ones need to address their concerns of choosing a treatment strategy that will harmonize with their worldview while grappling with state-of-the-art treatments versus alternative treatments. When I was asked who’s going to be my target audience, the obvious answer was everyone. It’s a rare person that has not had cancer touch their lives, either as a patient, a family member or friend. If you’re that rare person that hasn’t had cancer touch their lives, almost certainly at some point, cancer will drag you into its maelstrom. I hope that you find this show both a resource and a comfort in dealing with your cancer journey.
Dr. Gary Onik [00:02:21] I want to welcome Dr. Howard Freedman. He’s a retired pediatric ophthalmologist who lives in Naples Florida. Dr. Freedman is renowned for his pioneering work in inventing a quick and low-cost way for screening children as young as six months for amblyopia, one of the most prevalent causes of blindness in children, and his philanthropic work with the Lions Clubs to bring this advance to as many children as possible. Dr. Freedman is a friend of mine for over 45 years. He has quite an amazing story to share with us about his unique cancer journey, and I’d like to welcome Dr. Freedman to this podcast. Hello, Howie.
Dr. Freedman [00:03:08] Hello Gary. Nice to talk to you again.
Dr. Gary Onik [00:03:10] I’d like to start with your story of inventing this method for diagnosing amblyopia in children because I think that it really does illustrate some of the issues you have to deal with when trying to bring a new technology on board. Just tell us. Start out with what’s amblyopia? What did your invention do?
Dr. Freedman [00:03:34] Amblyopia is a Greek term that talks about lazy eye, and in the case, when a person does not have a good vision because of an abnormality in the brain that turns off the input from the eyes and it occurs early in life, and it is eminently treatable before age nine. So, if you pick it up early and correct the problems that are underlying it, which are usually three major problems, one is the kids have a bad refractory or they’re out of focus, or two they have a cataract or something that blocks the view into the eye. Or three, is they have a cross eye or a misaligned eye. Those are the three major cause of lazy eye or amblyopia. And as a pediatric ophthalmologist, I started in practice back in 1979 in Redwood Washington, and in practice, I remember seeing a number of kids. For example, there was a John who was an eight-year-old boy who came into my office, and he was twenty-four hundred in his right eye and twenty- twenty in his left and the right eye was much more far sighted than the left side and had never been in focus. And at that point in time, the best vision I could get him to was about 20-100 with glasses. And I said, you know, gosh, it’s really a shame that a child like this has a lazy eye that didn’t get picked up in school or in school screenings or anything else like that. And now at age eight and nine years old, is well into the area where the brain is set in its ways, so, the division can’t get really much better with time. We passed and got him a couple lines better, but he really never had good vision. Amblyopia is the largest cause of unilateral vision loss in America because it’s not picked up early. And it got my attention that as a pediatric ophthalmologist, we had a condition. If we can pick this up at age three or four, it would cure it because the brain is much more flexible and responsive to therapy at that age. So, I said, we need to start screening kids early, and that was what became my interest in amblyopia and early detection process.
Dr. Gary Onik [00:05:46] How did you go about trying to solve that problem?
Dr. Freedman [00:05:50] Well, I attended a conference in England and I found that a company had started a new technology of trying to screen kids with a new camera that they developed that was the size of a refrigerator to screen kid’s eyes. And in the next room, there was an inventive young ophthalmologist from Finland named Kerry Katona, who had put a special lens on one of his cameras and was able to now take a picture of the eye with his camera and do the same job. And I said, that’s a much better idea, but it needs to be Polaroid because we want to see it right away, rather than be at that point in time film, which is in the mid 80s. So, I went home thinking about this, and at a conference I went up to the Polaroid booth and I said, I’ve got an idea. Why don’t we make a camera that uses a Polaroid film to do this? And they said, we don’t do this. We sell millions of cameras, but we can lead you to our division that looks at experiments outside of our normal range called the OEM division. They helped me out with that and I met with some people in Cambridge, Massachusetts who were ex Polaroid engineers that they introduced me to. And I went into them and said, look, I’ve investigated this technology, and here’s how I think it will work. But I’d like to make into a Polaroid camera. I said, can you do this? And they said, sure, and I said, thank you very much. We shook hands, walked away, and about six months later, a big box came and it had my first screening camera 10 by 10 inches, and I took it to the office and Polaroid was very nice, they gave me as much film as I wanted. And I started testing the camera in the office on the kids, and it worked, and I was really surprised. It was nice. Essentially over the next two or three years we invented a smaller camera that worked better and actually got a patent on it. And eventually I sold the camera. I didn’t sell it, I sold the rights to the camera, the royalty, to an inventor company called Medical Technologies Inc., and they began producing the camera as the first commercial photos creator and it used Polaroid technology. I did a study on it; I did a paper on it; and it turns out it worked. And then I went to present it to my colleagues in pediatric ophthalmology, say, hey, I’ve got this new technology, it really works. And I said, we’ll be able to use it on all the kids, and it actually got no interest and actually got blocked by a lot of my colleagues who said, yes, you know, it’s a nice technology, but we need to study it further.
Dr. Gary Onik [00:08:24] To back that up. It was low risk. I mean, it was, it wasn’t like you were doing anything that could hurt somebody. It should have been something that they would have been happy to try.
Dr. Freedman [00:08:34] But many of my colleagues are researchers, and to them, they get funded to do research, and I understood why they wanted to do more research on it because they can improve their careers in doing something like that. For me, it was, hey, I do get a royalty on it and there was a financial incentive to sell cameras. But really, I was into it because I wanted to cure lazy eye. And it was an uphill battle to get it approved and to go through all the process of getting a [inaudible] and getting people to approve it. It was interesting that it was a tremendous process that took over 20 years before it became a recognized product that is now being used and became digital product. I had an interesting story during that period of time that we were in this development project and trying to sell the cameras, the company made an arrangement with a company called Pearle Optical, who had optical stories all over the nation, and he got an agreement with Pearle Optical after they did a pilot project in Chicago, showing that when they put it in their offices there, that the parents just loved it, they brought their kids in, the grandparents came in, they increased the business by 40 percent. And so, Pearle said, we want to take this and do it nationwide and put it in 6,000 of our stores all over the country. This is back in the 1980s. And they signed a contract with Medical Technology Inc. and they ordered the cameras and they were delivered and about ready to be distributed when they stopped. They put them in their warehouses and wouldn’t send them out. The company that owned them, which was named Luxottica, which sold glasses to optometrists, was contacted by optometrists and there was a feud between two types of optometrists. One type is in optical shops and the other one is in private practice, and they’re both working for the same principle of taking care of people and making money. But the ones in the private practice, were afraid that the business increase in the optical shops with the camera use would take away their business. And so, they said to Luxottica, we’ll stop ordering your lenses if you put these cameras in your office. Luxottica said, we make more money selling lenses and we will you know, in our offices. And they essentially told the company the camera doesn’t work, so we’re not going to use it. And they got sued and they lost, um, and they had to pay MGI a royalty payment or a settlement payment for it. I never got a penny of the money.
Dr. Gary Onik [00:11:12] But at the end of the day, it didn’t get out there to help.
Dr. Freedman [00:11:15] It didn’t get out. And a lot of people, my biggest concern was that, was that thousands of kids lost vision because they weren’t detected early when they could have been, if it had gotten out into the public at that point in time and gotten established. And to me, that’s real health care tragedy that could have been avoided, but understood the interests of each individual and it was all economic.
Dr. Gary Onik [00:11:42] There’s so much to learn from that story that pertains to the world of oncology and the oncologic patient, that it basically says the same basic forces that you ran up against with an eye innovation that could have helped tens of thousands of children. Those same forces trying to stop us. When I came up with the idea of just treating a portion of a prostate. Focal therapy, which interestingly enough, 20 years later is now… 20 years seems to be the time it takes to get something good going here, that I had members of the urologic community actually say I should be arrested for doing that because everyone up to that point treated the whole gland. And so, I think we see that with the academic community. We see that with the companies that we have to deal with in the pharmaceutical industry. It’s very interesting [inaudible] that these are basic problems not peculiar to one area of medicine, but peculiar to medicine in general, when you’re trying to change the way things are done and it’s expected. And so, I don’t take it personally anymore. I’m glad I wasn’t arrested. But, you know, I think that it’s something that right now I’m dealing with every day. So, what I’d like to do is segue from that and talk about how your experience in cancer affected your life.
Dr. Freedman [00:13:23] I fought cancer before and fortunately overcame it the first time. I’m doing the same thing the second time, thanks to you. The first episode was when I got Hodgkin’s disease in 1979. I had just gotten married about two weeks before and I got diagnosed in St. Louis at Barnes Hospital with advanced Hodgkin’s disease that had spread from my spleen all the way up into my chest, into my neck. And at that point in time, it was a death sentence back in 1977, with only a few months to live. At that point in time, I didn’t know what the other options were. Well, the people of St. Louis, when I asked the doctor who was the head of the oncology department while I was in the hospital after having chest surgery the doc made the diagnosis, I said, where’s the best place for me to get treated? And he said here. And I said, I know you got a good program, but where’s the best place to get treated? And he said here, I said oh, thank you very much and turned to my wife after he left. I think this was the time when I had to take charge of my care because you can’t trust doctors to have your own best interests. Because I eventually found out that the best place to be treated, which was told to me by my medical school colleague who was a resident oncology at NIH, who’s now the director of the Cancer Center in NIH. And he said, well, Howie, we’ve got a really good program here. The person who has the best treatment for this with the best results is in Stanford named Saul Rosenberg. And I said, What’s his phone number? And he gave me his phone number. And so, I went there. This is a second opinion. I got another opinion from my colleague in Harvard that I trained with, who said, you know, NIH or Stanford were the best programs. So I went to Stanford, got on a plane right out of the hospital, and I went to Saul Rosenberg and Henry Kaplan, who were doing innovative treatments for Hodgkin’s disease at that time and were actually curing patients that had never been cured before, primarily with radiation therapy. And they combined chemotherapy and radiation therapy together. I entered their program and it turns out that it cured me. And now, 43 years later I’m still in remission from my Hodgkin’s disease. The interesting story was I was sitting in the waiting room, and I was talking to a gentleman right next to me and I said where you’re from? St. Louis. And I said what you got? Hodgkins. Turns out he has the same type and stage as me. And I said, why are you here? He said, well, they almost killed me in St. Louis. I said, why? They weren’t going to take my spleen out of which I had taken out at Stanford, and were going to radiate it. And my platelet count got so low I almost bled to death. And I said, oh, I’m sorry to hear that. So, he is now at Stanford to get treatment. And I never heard about until 40 years later, what happened to him. And it turned out he died the next year because he got in too late. And I was very lucky because I said to myself that would have been me If I had gone to St. Louis and they had done the same thing to me. So, it turned out to me that my ability to be able to search out the best program and the best treatment option, really helped me because it allowed me a path to recovery and a successful treatment. And to me, I think that’s the message. Always get a second opinion, not you know, don’t trust your doctors, but always trust but verify; verify where the best place is to get the best treatment.
Dr. Gary Onik [00:16:57] You know, patients are in a really difficult situation right now because they have to do exactly what you’ve said. They have to do some of their own research because they are not necessarily getting what might be best for them. We see this all the time with prostate cancer patients, where patients who might have very aggressive prostate cancer, who… an operation would not work well, where they might leave the cancer behind, get positive margins and leave the cancer behind, where they’re getting those operations, when they should be getting some other well-known treatments that work very well in those instances, but are not necessarily done by every institution. So, it’s a real problem. I don’t think that there’s a single good answer for patients except to get a number of opinions. Maybe you can look online and see what the options are and then, you know, explore those with the doctors that you trust. So, we come now and we are 45 years later and we’ve had contact during those years. We’re both, you know, sailors and interacted over that time. And then you get another diagnosis. And can you tell us what happened and particularly how you felt about it, suddenly getting another diagnosis with probably a similar prognosis?
Dr. Freedman [00:18:34] They told me back at Stanford that one of the side effects, of two side effects of therapy is I could get heart disease later or I could get a secondary cancer. Well, I did get the heart disease and had open heart surgery, and I was really lucky because it took 43 years before the secondary cancer came out and late out last summer, about August or September I just wasn’t having a good appetite, and I decided I had something going on with me and I took a feeling into my belly and I felt that I had a little tumor there inside my belly and went to my GI doc. And I said, I need a scan, I need to find out what’s going on with me. And it turned out it was a metastatic cancer that had developed in the middle of my abdomen, and it had spread to my liver. And that spread, being metastatic put me into what they call stage four, which is, well, advanced cancer. And as I looked up the information on this type of tumor, which is a sarcoma, which is a soft tissue tumor and then spread, the life expectancy was six months to a year. And I said, well, that’s not really good. I was really kind of pissed because I really wanted a lot more time, but I didn’t really seem like I was getting a chance for that. I had a really good life, I’ve accomplished a lot of things, so I didn’t have a lot of regrets, but I still was doing a lot of good things for volunteering, um, and I just didn’t want to die. So, I said what do I do? So, I investigated all the possibilities. I went to my oncologist who had been taking care of me for years after my Hodgkin’s disease and went up to a cancer center in Florida and got an opinion from the cancer center about what to do. And they said to me [inaudible] you need to get chemotherapy. And I said, the drugs or the chemotherapy cause heart problems and I’ve got heart problems. I really don’t want to take that. Is there any other type of therapy like immunotherapy that you do? And they said, well, you know, we’ve got two protocols here which you have to go through chemotherapy first before you can get it. And I said, well, that’s not good. What I really want is immunotherapy because I looked into it and I know that there are some good advances in that for many other cancers. And the later doctor said, well, we’d like to have it, but maybe we’ll get it in six years. And I said, thank you very much. And I went on, I said to my wife, geez this is really frustrating, I’m really disappointed because this is not the kind of answer I wanted. I wanted someone to tell me, what’s the best innovative way? What are my options, etc., etc.? So, at that point in time, I reached out to some of my friends who were specialists like Dr. Doroshow, who heads, is the deputy director of the cancer institute and he gave me good advice, gave me some people to talk to, and I couldn’t find any program that was going to really help me, except for yours. And I had been following what you had been doing with prostate treatment, with cryotherapy, which was incredibly innovative and was really reformative. And then heard, as we talk, that you had been getting into doing a cancer vaccine, doing cryotherapy as well as immunotherapy directly into cancers. And I said that makes good sense. That’s what I want. And we had the discussion about what to do. And fortunately, you said, yes, I can do you. And that saved my life. Thank you.
Dr. Gary Onik [00:22:13] I think when I see and I talk to patients, I use a rule, and I call it my medical golden rule, basically, I say to myself, if I was in that patient’s position, would I want this treatment? And if I come up with no, then then that’s not something I should be doing to somebody, you know, unless I’m willing to have something, then I don’t think that I should be doing it to anyone else. I think it was a rather easy decision to say, let’s give this a try. I was quite amazed because we are saying in medicine, the enemy of good is better. And so of course, I tried to do everything better and in point of fact, it made things more complicated. We don’t have to go through those. It reminds me the story of my, my mother. She had colon cancer, and when she was having resection of the colon cancer and I sent her to the best guy. I knew him, I had worked with him doing liver cancer treatments. And he treated her, by the best guy, and she got sick afterwards, and he had left a sponge in her. And he felt absolutely awful. I don’t know why that happened, but more than likely he was distracted by trying to do some extra things that, you know, he didn’t need to do. So, I was quite amazed when we looked at your scan four weeks later and the abdominal tumor was gone. I mean, that was one of the most wonderful moments in my medical career that we could see that happen, and we’re still working on the liver, but we’re going in the right direction and I’m very, very hopeful that we’re going to get a complete response. The last thing I want to ask you Howie is where did you get the strength from and where did you and Pam, your wife, get the strength from to deal with these, these major upheavals?
Dr. Freedman [00:24:23] Well, I got to tell you, it was one of the best days of my life when I saw the PET scan where my abdominal tumor, not just in my abdomen buy my pelvis, had disappeared, and the other tumors. And the second scan that I got showed that after the radiation treatment that you led me into with the Y-90 particles had worked also to help reduce the tumor. So, I’m hopefully on the way to reducing the tumor and my, sort of, fingers are crossed for a long-term remission or cure. But how do I react to that? That’s a really good question. Um, I think in life you always have to think positive. And although I fully realize that and I got my affairs in order realizing I could die and I’m saying, look, if I could get more time that would be really nice. And we entered this way saying, you know, we accept the inevitable, and I’m 74 years old. I’ve had a really good life, but I would certainly like more. It involved four or five different areas. One is spiritual, you know, being positive, you know, asking my friends to pray for me, which they did. And I really think that that always, always helps, having a really positive mental attitude. I remember doing meditation when I was getting my first cancer treatment, visualizing my body’s immune system, fighting my cancer off. I don’t know if that worked or not, but it couldn’t hurt. So, I did the same thing now. So, every night I enter into a meditative state and I start to visualize internally trying to get my cancer better. It led me into doing some supplements that seem to help. One of the best things is when you got me to do a study in Europe that looked at my cancer in much more details than the studies that I had done the United States. And although it was excessive, it came back with a whole lot of different information. And it turns out that the tumors that I had, were responsive to a couple of the chemicals that you put in for checkpoint inhibitors, which was the basis for why it works and it’s continuing to work very well. And that gave me hope and hope was really a nice thing to have. I haven’t had a sick day since I got diagnosed. If I had gone through chemotherapy I would have had months of feeling bad. I’m very, very lucky that I was able to pick an alternative and find an alternative therapy. And I think those are the internal issues. And just for your approach every day on a positive basis and continue a normal lifestyle and enjoy golf and all the other things. But I’m really appreciative to you, because I think you have a policy and a procedure that can really benefit people. And it’s unknown, and it’s not well-respected and it’s not admired because most people have not done it before. And we have inertia in medicine that says, I don’t do that, and, you know, I don’t see enough studies on it, and therefore I’m not going to do it. It’s very interesting when I get back to my cancer specialist Moffitt, and she’s looked at all the results and being a naysayer. Last month, she said to me, you know, I think we might have to look in a different way of doing things. I’m going to present this to my conference or my colleagues because maybe we’re missing something that we should be doing. To me, that was music to my ears, that someone from the establishment who was involved with just protocols and doing chemotherapy based on drugs that pharmaceutical companies were paying them for, now says, you know, maybe doing immunotherapy, personalized basis like what you did, really will help other people and cancer should, make more cancer survivors. And to me, that’s the biggest hope I have, is the example that you have set here with me, will be able to reach out to many other doctors to say, yes, we can look at other alternatives rather than just the traditional stuff we’re doing, and really give people the hope and possibility of using the new technology and new techniques to help out their cancer.
Dr. Gary Onik [00:28:35] Howie, thank you very much. At some point, I’d like to get you back and talk about these other issues going through FDA studies. We’re trying to do things responsibly and we’re trying to check all the boxes. There are always issues to deal with. I have found that the funding issue and it didn’t seem like you had that issue, but the funding issue can be a real difficulty as well. And dealing with the Big Pharma can also be a very big issue. But I want to thank you so much for coming on and sharing your story and you said a lot of nice things about me. You know, your payment is coming in the mail for that, and hopefully have many more years to do the things we want to do and some of them together.
Dr. Freedman [00:29:31] Thank you, Gary, and I wish you all the best of luck in getting your ideas out to the mainstream community and to people, so that more people can be helped like you help me. Thank you so much.
Dr. Gary Onik [00:29:42] Thank you.
Dr. Gary Onik [00:29:59] Well, this is the segment of the show where we highlight new advances in both cancer treatment as well as cancer policy. Today, I’d like to talk to you about a very hopeful bill that’s been passed by Congress, which is called the New Cures 2.0 bill. What this does is it links FDA approval to Medicare payment. At the present time before this bill linked the two, you could get an FDA approval of a device and it wouldn’t be paid for. So therefore, the approval was of little value if the patients had no way of paying for it. This bill is really proof that when the government wants to help, they can do something really good. And so, these two are linked, both approval and payment approved by the FDA, payment by Medicare. And the approval and this linkage goes for at least four years until Medicare looks at what is going on and that it is efficacious and good for patients. So, another hopeful thing actually coming from government.
Dr. Gary Onik [00:31:30] This is the part of the podcast where we go to the mailbag and listeners get to ask us questions. Please don’t send in any questions that deal with specific medical information for you or one in your family, because there’s no way that I can give you a reasonable answer to a specific medical question because I just won’t have enough information and that would be wrong of me. So general questions relating to your journey and cancer are more than welcome. So, let’s go to today’s question. Janet from Illinois asks: “My mother has cancer that has spread to her bones. A friend of mine told me about a cancer center in Mexico that is getting results with natural therapies. I’ve looked at their website and the testimonials by their patients are very impressive. How do I know that they are on the up and up and credible? And I will not be wasting my money by sending my mother there?” Well, it’s an interesting question. First off, just because they’re in Mexico doesn’t mean that they’re not credible. If we are talking about a U.S. doctor who does work in Mexico, the first thing I would ask is, why isn’t he doing that work in the United States? What’s the reason? Is he using medications that are not FDA approved, and therefore he has to use them down in Mexico? I’ve got a personal story associated with that. I had a patient with an immunotherapy regimen, and he did get a response, but then the response tapered off and I brought him to Orlando to meet with… he had colon cancer, and I brought him to Orlando to meet with a specialist in colon cancer. He assessed the situation for my patient, and basically, the tumor had regressed enough that he was now resectable. He now could have the cancer removed. Great result. The patient pursued more immunotherapy and went to a program down in Mexico to get that immunotherapy. The first problem I had with that was, that this is a curable patient now. You know, my view and when we do immunotherapy, is that if a patient has a traditional curative option, then that’s what they should be doing unless there is some really extenuating circumstance. That patient went down there, had the immunotherapy and he passed away three days later after having this therapy, used medications that are not approved in the United States, but it pointed up to me that we have to be very, very careful going outside the United States and using medications that are not approved within the States. The next thing that I would say is that the best approach to finding out if something is credible, is look in the literature. If you have a physician in a clinic down in Mexico who is saying we’re getting these wonderful results and they have testimonials, what you should do is get one of your physicians or physicians or one of your friends who is very facile with the internet and go on Medline or PubMed, which talks about and shows you the literature, and you can put a physician’s or researcher’s name into PubMed and see all of the research that has been done and the results that they’ve published. If you put a researcher’s or a physician’s name in, who is touting a center with these marvelous results, if they haven’t published those results, then you can’t believe them. Number one, it’s their responsibility to publish those results if they’re that good so that other physicians can explore the same possibilities in terms of patient treatment. But it’s important that they’re looking at the results. It’s amazing how physicians can think they’re doing well in one area until they look at their data and find out that they’re not. Particularly true of complications. When I was doing spinal surgery, a long time ago, I was a professor of neurosurgery before I went into strictly cancer. There was a complication when you did spinal surgery of where you actually doing the spinal surgery, you injured the aorta or injured the vena cava. And patients, you know, it’s a life-threatening injury, you know, patients can bleed to death. Well, you know, that occurred in about 1 in 500 cases. If you’re a practicing surgeon and you’re doing 50 spines a year, then you’re not going to see that complication for 10 years, and you’re going to say that complication never happens. But when you look at things as a group, as a, as a population, those things do happen. Lastly, you should know that if a medication is approved in the United States by the FDA, that medication, and let’s say it’s approved for breast cancer, that medication, if your physician feels can be efficacious for you and you have prostate cancer and it’s not approved for prostate cancer, your physician is allowed by law and is actually encouraged by the FDA to use it, what we call, in off-label fashion. That is a very reasonable thing to do, but it’s very different than using a medication that has never been approved for anything because the safety aspects were not carefully evaluated. You have to be careful when you go to places and clinics outside the United States.
Dr. Gary Onik [00:38:38] If you would like to ask us a question for the mailbag, you can go to garyonikmd.com. There is a contact form that you can fill out that will be forwarded to us, and we’ll consider your question for our show. Thank you for listening to our podcast. I hope that it provided you with some useful information, some hope and some comfort. Thank you very much.